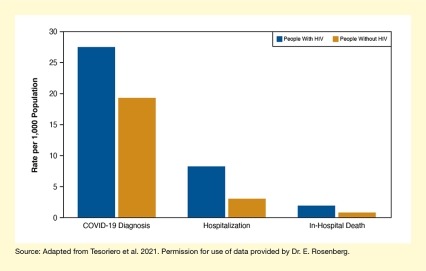
This study found that:
- In New York State, people living with HIV were more likely to be diagnosed with, hospitalized for, and die in hospital from COVID-19 than were people without HIV.
- People with more advanced HIV disease faced even greater risks from COVID‑19.
New York State has long been an epicenter of the U.S. HIV epidemic, and initially it was also an epicenter of the COVID-19 pandemic. Because HIV increases vulnerability to other infections, Dr. James M. Tesoriero and colleagues from the New York State Department of Health in Albany and the State University of New York, Rensselaer, investigated whether people living with HIV were more susceptible to coronavirus infection and to more severe COVID-19 disease than people without HIV. Their study demonstrated that compared with peers without HIV, people with a prior diagnosis of HIV in New York State were more likely to have a COVID-19 diagnosis, require hospitalization, or die from the disease during the first phase of the COVID-19 pandemic.
HIV Diagnosis Increases Risk of Severe COVID-19
The association of HIV and coronavirus infection had already been investigated in small studies of hospitalized patients with COVID-19. In this study, however, Dr. Tesoriero and his team linked information from state-wide databases recording HIV diagnoses, laboratory diagnoses of COVID-19, and hospitalization records to compare COVID-19–related outcomes of people with and without HIV among the entire population of New York State. Their analyses included data for more than 108,000 people previously diagnosed with HIV and more than 19.3 million people without HIV. Among these, almost 3,000 people with HIV and about 375,000 people without HIV were diagnosed with COVID-19 between March 1 and June 7, 2020.
The analyses revealed that people with HIV were 43 percent more likely to be diagnosed with COVID-19, 161 percent more likely to be hospitalized with COVID-19, and 155 percent more likely to die in hospital with COVID-19, compared with those without HIV (see Figure). After adjusting for demographic factors, people with HIV had similar COVID-19 diagnosis rates as those without HIV but were more likely to have severe disease. “The likelihood of developing severe COVID-19 that required hospitalization appeared to explain elevated levels of hospitalization and death; persons with HIV still had 1.38 times the level of hospitalization compared to those without,” explains the study’s principal investigator, Dr. Eli S. Rosenberg. The findings are consistent with other studies showing that, compared with other populations, people living with HIV seem to experience more severe COVID-19 disease, but have similar outcomes once hospitalized.
Additional analyses identified subgroup differences among people with HIV. Blacks and Hispanics were more likely to receive a diagnosis of COVID-19; however, those who had COVID-19 were not more likely than Whites to have severe disease. Finally, the risk of hospitalization was greater the more advanced HIV disease was (i.e., the lower CD4+ T-cell counts were).
“Our results indicate that this population has experienced an increased burden of COVID-19 and requires particular attention from the clinical and public health communities,” says Dr. Rosenberg. What remains to be determined is the degree to which the increased COVID-19 severity is directly due to HIV rather than to other co-existing conditions or social factors associated with HIV.
This research was supported by NIDA grant DA051302.
- Text Description of Figure
-
This bar chart shows the differences in COVID-19–related outcomes in people with and without HIV in New York State. Blue bars represent people living with HIV and gold bars represent people without HIV. The vertical y-axis shows the rate per 1,000 population on a scale from 0 to 30. The left pair of bars indicates the rate for COVID-19 diagnosis; it was 27.7/1,000 for people with HIV and 19.4/1,000 for people without HIV. The middle pair of bars shows the rate of hospitalization for COVID-19; it was 8.3/1,000 for people with HIV and 3.2/1,000 for people without HIV. The right pair of bars represents the rate of in-hospital death from COVID-19; it was 1.9/1,000 for people with HIV and 0.8/1,000 for people without HIV.
Source:
- Tesoriero, J.M., Swain, C.E., Pierce, J.L., et al. (2021). COVID-19 Outcomes Among Persons Living With or Without Diagnosed HIV Infection in New York State. JAMA Network Open, 4(2), e2037069, 2021.