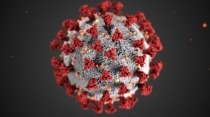
As people across the U.S. and the rest of the world contend with coronavirus disease 2019 (COVID-19), the research community should be alert to the possibility that it could hit some populations with substance use disorders (SUDs) particularly hard. Because it attacks the lungs, the coronavirus that causes COVID-19 could be an especially serious threat to those who smoke tobacco or marijuana or who vape. People with opioid use disorder (OUD) and methamphetamine use disorder may also be vulnerable due to those drugs’ effects on respiratory and pulmonary health. Additionally, individuals with a substance use disorder are more likely to experience homelessness or incarceration than those in the general population, and these circumstances pose unique challenges regarding transmission of the virus that causes COVID-19. All these possibilities should be a focus of active surveillance as we work to understand this emerging health threat.
SARS-CoV-2, the virus that causes COVID-19 is believed to have jumped species from other mammals (likely bats) to first infect humans in Wuhan, capital of China’s Hubei province, in late 2019. It attacks the respiratory tract and appears to have a higher fatality rate than seasonal influenza. The exact fatality rate is still unknown, since it depends on the number of undiagnosed and asymptomatic cases, and further analyses are needed to determine those figures. Thus far, deaths and serious illness from COVID-19 seem concentrated among those who are older and who have underlying health issues, such as diabetes, cancer, and respiratory conditions. It is therefore reasonable to be concerned that compromised lung function or lung disease related to smoking history, such as chronic obstructive pulmonary disease (COPD), could put people at risk for serious complications of COVID-19.
Co-occurring conditions including COPD, cardiovascular disease, and other respiratory diseases have been found to worsen prognosis in patients with other coronaviruses that affect the respiratory system, such as those that cause SARS and MERS. According to a case series published in JAMA based on data from the Chinese Center for Disease Control and Prevention (China CDC), the case fatality rate (CFR) for COVID-19 was 6.3 percent for those with chronic respiratory disease, compared to a CFR of 2.3 percent overall. In China, 52.9 percent of men smoke, in contrast to just 2.4 percent of women; further analysis of the emerging COVID-19 data from China could help determine if this disparity is contributing to the higher mortality observed in men compared to women, as reported by China CDC. While data thus far are preliminary, they do highlight the need for further research to clarify the role of underlying illness and other factors in susceptibility to COVID-19 and its clinical course.
Vaping, like smoking, may also harm lung health. Whether it can lead to COPD is still unknown, but emerging evidence suggests that exposure to aerosols from e-cigarettes harms the cells of the lung and diminishes the ability to respond to infection. In one NIH-supported study, for instance, influenza virus-infected mice exposed to these aerosols had enhanced tissue damage and inflammation.
People who use opioids at high doses medically or who have OUD face separate challenges to their respiratory health. Since opioids act in the brainstem to slow breathing, their use not only puts the user at risk of life-threatening or fatal overdose, it may also cause a harmful decrease in oxygen in the blood (hypoxemia). Lack of oxygen can be especially damaging to the brain; while brain cells can withstand short periods of low oxygen, they can suffer damage when this state persists. Chronic respiratory disease is already known to increase overdose mortality risk among people taking opioids, and thus diminished lung capacity from COVID-19 could similarly endanger this population.
A history of methamphetamine use may also put people at risk. Methamphetamine constricts the blood vessels, which is one of the properties that contributes to pulmonary damage and pulmonary hypertension in people who use it. Clinicians should be prepared to monitor the possible adverse effects of methamphetamine use, the prevalence of which is increasing in our country, when treating those with COVID-19.
Other risks for people with substance use disorders include decreased access to health care, housing insecurity, and greater likelihood for incarceration. Limited access to health care places people with addiction at greater risk for many illnesses, but if hospitals and clinics are pushed to their capacity, it could be that people with addiction—who are already stigmatized and underserved by the healthcare system—will experience even greater barriers to treatment for COVID-19. Homelessness or incarceration can expose people to environments where they are in close contact with others who might also be at higher risk for infections. The prospect of self-quarantine and other public health measures may also disrupt access to syringe services, medications, and other support needed by people with OUD.
We know very little right now about COVID-19 and even less about its intersection with substance use disorders. But we can make educated guesses based on past experience that people with compromised health due to smoking or vaping and people with opioid, methamphetamine, cannabis, and other substance use disorders could find themselves at increased risk of COVID-19 and its more serious complications—for multiple physiological and social/environmental reasons. The research community should thus be alert to associations between COVID-19 case severity/mortality and substance use, smoking or vaping history, and smoking- or vaping-related lung disease. We must also ensure that patients with substance use disorders are not discriminated against if a rise in COVID-19 cases places added burden on our healthcare system.
As we strive to confront the major health challenges of opioid and other drug overdoses—and now the rising infections with COVID-19—NIDA encourages researchers to request supplements that will allow them to obtain data on the risks for COVID-19 in individuals experiencing substance use disorders.
Additional Links
- Coronavirus.gov
- Coronavirus Disease 2019 (COVID-19) (CDC)
- Latest Research Information from NIH
- COVID-19 Information from NIDA
- COVID-19 Information from SAMHSA
For those with questions about how their state justice systems are adjusting operating procedures in response to COVID-19, The Marshall Project is tracking changes as they occur. Also, the Vera Institute of Justice has developed guidance for justice system adjustments to COVID-19.