A new modelling study suggests that when patients who inject opioids continue an antibiotic treatment for infective endocarditis outside of the hospital, they experience better long-term health outcomes than patients who receive the standard four to six weeks of inpatient, intravenous antibiotic therapy. In addition to reducing infective endocarditis-related deaths and extending life expectancy, this analysis suggests that these outpatient strategies are more cost-effective than the standard approach. The study was published today in JAMA Network Open and funded by the National Institute on Drug Abuse (NIDA), part of the National Institutes of Health.
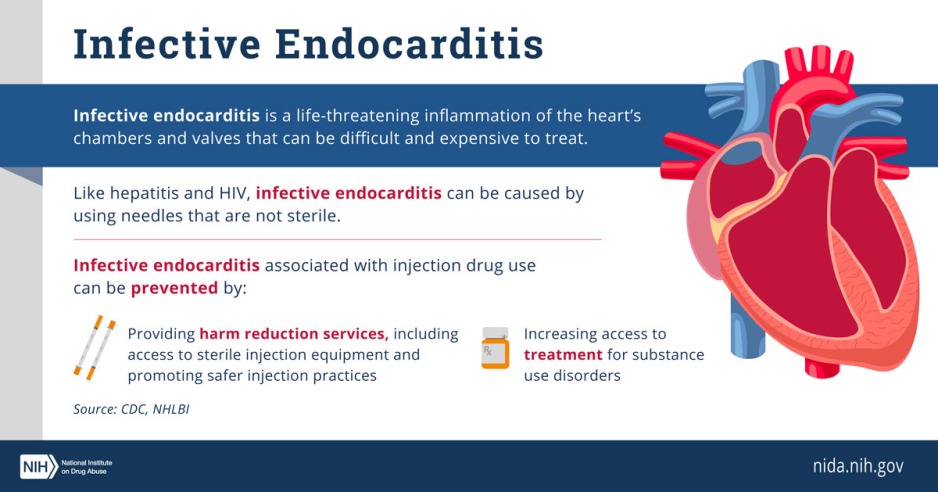
Endocarditis is a life-threatening inflammation of the heart valves. One in 10 hospitalizations for endocarditis is associated with injection drug use, and these numbers continue to rise. Many drugs can be taken via injection, including cocaine, methamphetamine, and opioids like heroin and fentanyl. Inadequate access to sterile injection equipment is common, and dramatically increases risk of infection in people who use drugs.
Though more immediately fatal than HIV and hepatitis C virus, which are also spread by injection drug use, endocarditis is not as well-known. Research estimates that if current trends continue, more than 250,000 Americans will die of drug use-associated endocarditis from 2020 to 2030.
“Endocarditis is one of the numerous harms associated with injecting drugs,” said NIDA Director Nora. D. Volkow, M.D. “Developing effective, patient-centered treatment for this potentially fatal condition is critical. It is also imperative to embrace and implement harm reduction strategies, such as syringe services programs, which we know can help prevent endocarditis in the first place.”
Researchers at the University of Colorado School of Medicine, Denver, and Boston Medical Center sought to better understand the effects of different treatment strategies for drug use-associated endocarditis, a serious condition that can lead to death. To properly treat this condition, patients often need weeks of inpatient intravenous antibiotic therapy or, in some cases, heart surgery. This lengthy treatment regimen presents hospitalized patients with physical, mental, financial, and social challenges. Twenty percent of patients admitted with drug use-associated endocarditis leave the hospital before completing treatment. Very few patients – less than 8% – are subsequently connected with addiction care services that provide further healthcare and support upon discharge.
These factors highlight a pressing need for alternative therapies that shorten hospitalization time or allow patients to complete treatment even after they leave the hospital. Prior studies have demonstrated that intravenous or oral antibiotics that patients can take at home or in community-operated health facilities are as safe and effective as inpatient intravenous antibiotics. However, there are few investigations into these alternative treatment strategies, largely because of stigmatized beliefs about people who use drugs and their potential misuse of treatment catheters, or PICC lines, used to administer intravenous treatments.
Led by Joshua Barocas, M.D., associate professor of medicine at the University of Colorado School of Medicine, Denver, researchers investigated the efficacy of outpatient treatment for infective endocarditis. They created a robust model that simulated the natural history of injection opioid use in 5 million individuals. The population for this model had a mean age of 42 and were 70% male, reflecting the age and gender demographics for the U.S. population who inject opioids, informed by previous studies and the U.S. Census.
The researchers compared life expectancies, rates of treatment completion, endocarditis and overdose deaths, and average costs across four treatment strategies in these individuals. Two of these treatment strategies offered the standard four to six weeks of inpatient intravenous antibiotics, either with or without inpatient addiction care services. The other two strategies provided three weeks of inpatient intravenous antibiotics and addiction care services followed by either outpatient intravenous or oral antibiotics.
Of note, the scientists accounted for socioeconomic challenges such as homelessness by assuming that only half of the hospitalized patients could receive at-home intravenous antibiotics.
In individuals hypothesized to contract infective endocarditis according to the model, the researchers found a substantial increase in life expectancy and reduction in deaths caused by endocarditis or overdose for individuals who received outpatient intravenous antibiotics, oral antibiotics, or inpatient addiction care services in addition to standard treatment compared to the standard approach. Of all four strategies, the addition of oral antibiotics and outpatient intravenous antibiotics led to the greatest cure rates (80.3% and 78.8%, respectively, compared to 77.6% for inpatient intravenous antibiotic therapy plus addiction care services and 77.6% for inpatient intravenous antibiotic therapy only).
The strategy that included outpatient intravenous antibiotics also cost less than any of the other strategies ($412,150 per person compared to $413,920 for additional oral antibiotics, $416,570 for inpatient intravenous antibiotics, and $416,990 for inpatient intravenous antibiotics and addiction care services). The researchers suggest that these strategies could save the healthcare system more than $6 billion in hospitalizations alone for the yearly estimated 750,000 Americans who inject drugs.
The researchers say these results should be tested in randomized clinical trials that do not exclude people who inject drugs from participation. They also emphasize the need for a national surveillance system for injection drug use-related endocarditis, based on existing surveillance strategies for HIV and hepatitis C. Expanding research in this area could strengthen evidence for patient-centered decision making when offering treatment strategies for endocarditis.
“Outpatient treatment approaches for endocarditis may not only save lives, but also save money that could then be allocated to evidence-based programs for the opioid crisis,” said Dr. Barocas. “These strategies include promoting safer injection and other harm reduction techniques, improving access to medications for opioid use disorder, and funding outpatient support systems. This would allow people who use drugs to not only heal from endocarditis but do so in a way that they can more easily return to work, to life, and to family.”
Reference: JW Adams, et al. Simulated cost-effectiveness and long-term clinical outcomes associated with strategies for addiction care and antibiotics for infective endocarditis related to drug use. JAMA Network Open. DOI: 10.1001/jamanetworkopen.2022.0541 (2022).
- View Infographic: Infective Endocarditis
NIDA Press Office
301-443-6245
media@nida.nih.gov
About the National Institute on Drug Abuse (NIDA): NIDA is a component of the National Institutes of Health, U.S. Department of Health and Human Services. NIDA supports most of the world’s research on the health aspects of drug use and addiction. The Institute carries out a large variety of programs to inform policy, improve practice, and advance addiction science. For more information about NIDA and its programs, visit www.nida.nih.gov.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®