About the NIH HEAL Initiative
The National Institutes of Health (NIH) Helping to End Addiction Long-term® Initiative or NIH HEAL Initiative®, was launched in 2018 to accelerate scientific solutions to the devastating addiction and overdose crisis in the United States. This NIH-wide Initiative is jointly led by the National Institute on Drug Abuse (NIDA) and the National Institute of Neurological Disorders and Stroke (NINDS).
NIDA leads HEAL research efforts concerning opioid use disorder (OUD) and opioid and other drug related overdoses, and research at the intersection of pain and OUD. NINDS, in collaboration with the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Center for Complementary and Integrative Health (NCCIH) coordinates HEAL research efforts across NIH Institutes and Centers, including NIDA, to develop safe and effective pain treatment and prevention strategies.1 In the day-to-day program leadership and management, virtually every NIH Institute, Center, and Office (ICO) is involved in some capacity, with 21 ICOs leading and managing different HEAL programs. HEAL collaborations also extend across the U.S. Department of Health and Human Services, community organizations, research institutions, and the private sector.
About the NIDA HEAL Strategic Plan
This Strategic Plan reflects research priorities that will inform the OUD and the opioid and other drug overdose arm of the HEAL Initiative led by NIDA. It was developed with input from the extramural scientific community and other NIDA stakeholders via a Request for Information (NOT-NS-24-106),2 and input from NIDA staff via institute-wide strategic planning discussions. This plan complements the broader body of research NIDA supports in service of its mission to advance science on drug use and addiction and apply that knowledge to improve individual and public health. The NIDA wide strategic plan is available here: 2022-2026 NIDA Strategic Plan.
Introduction
Since its launch with the support of Congress in 2018, the NIH HEAL Initiative has made the nation’s largest ever investment in research to end the national overdose crisis. To date, both NIDA and NINDS have administered a cumulative $3.9 billion to fund over 2,200 research projects in all 50 states and the District of Columbia and have driven innovative solutions to help address opioid use disorders, overdoses, and chronic pain by promoting collaborative science and data sharing, advancing implementation research laser-focused on improved patient care, and pushing the boundaries of rapid therapeutic and diagnostic development. NIDA has led more than half of this work, with an investment of $2.1 billion in 1,200 research projects since the inception of HEAL.
Drug overdoses in the United States started to rise beginning in the late 1990s, following increased prescribing of opioid analgesics to address the crisis from untreated chronic pain. Overprescription of these medications along with poorly managed pain, led to a growing problem of OUD and opioid-related overdose fatalities. Opioid overdoses accelerated after 2010, when people with OUD increasingly turned to heroin as a cheaper alternative to prescription opioids. This was followed by the influx of fentanyl – a very potent synthetic opioid, and more recently expanded into a polysubstance overdose crisis. Currently, fentanyl and other synthetic opioids other than methadone, frequently in combination with cocaine and methamphetamine, are driving overdose fatalities, which in 2023 led to 105,007 deaths.3
However, our collective national investment to curb the overdose crisis is producing results. The escalation of drug overdose deaths began to decelerate in 2021 and recent data from the Centers for Disease Control and Prevention show a steep decline beginning in 2023 and continuing into 2024. Nonetheless, overdose fatalities still account for tens of thousands of deaths annually4 and there are nearly 9 million Americans ages 12 and older who misused opioids in the past year, and an estimated 5.7 million with OUD, which is appraised to be an undercount.5,6,7 In parallel, chronic pain affects 50 million adults in the United States with nearly 20 million living daily with chronic pain that interferes with their lives and if improperly treated, puts them at risk for illicit opioid misuse alongside the risk of OUD and overdoses.8
The NIH HEAL Initiative will continue to address these challenges using a multifaceted evidence-based approach that brings together scientists, healthcare providers, patient advocates, community members, the private sector, and multiple levels of government – all sharply focused on developing and deploying scientific solutions with the ultimate goal of preventing all overdoses. Toward that goal, this Strategic Plan reflects NIDA’s commitment to ensure that HEAL-supported research will remain focused on efforts to accelerate scientific solutions to urgently address the overdose crisis and prevent it from happening again.
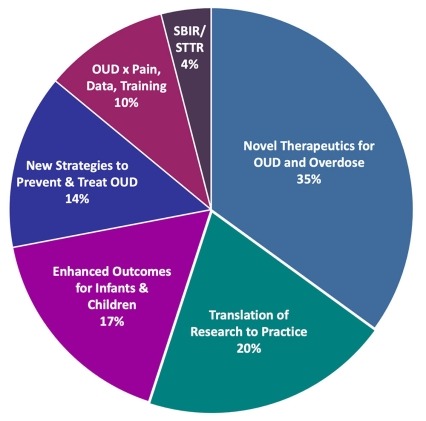
NIDA HEAL Profile (FY 2024)
Year Established: 2018
FY 2024 Budget: $355 million
FY 2024 Supported Investigators: >250
FY 2024 Newly Funded: Early-Stage Investigators: 16
FY 2024 Training Awards: >10
FY 2024 Funded Research Projects: >280
FY 2024 Research Focus Areas (% Budget)
- Novel Therapeutics for Opioid Use Disorders and Overdoses
- Translation of Research to Practice for the Treatment of Opioid Use Disorders
- Enhanced Outcomes for Infants and Children Exposed to Opioids
- New Strategies to Prevent and Treat Opioid Use Disorders
- Opioid Use Disorders x Pain, Data, Training (previously “Cross-Cutting”)
- Small Business SBIR and STTR Support
NIDA HEAL Research Priorities
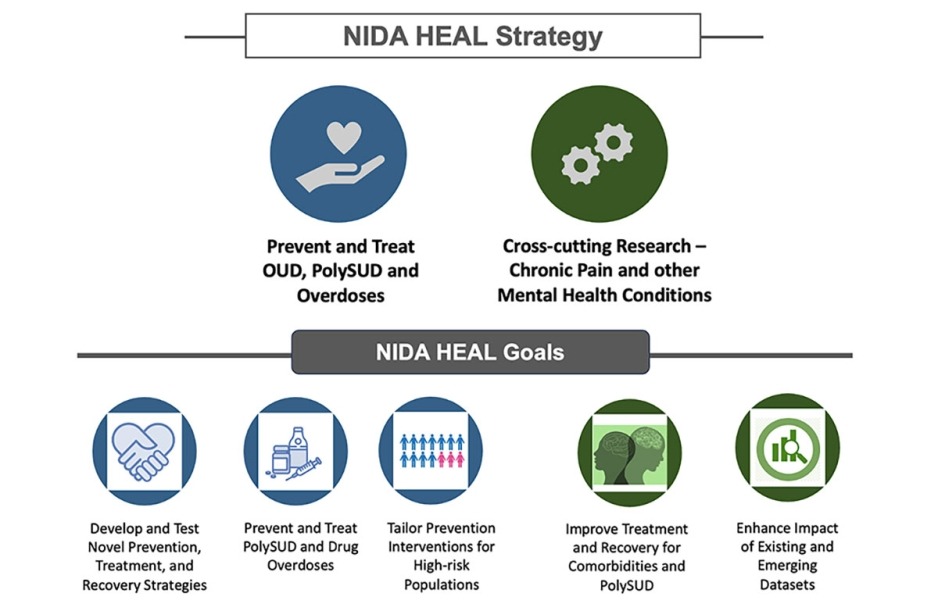
This HEAL Initiative strategic plan for OUD and overdoses includes two core research objectives around which NIDA will prioritize HEAL research investments over the next 5 years:
(1) Advance research to prevent and treat OUD and overdoses including from polysubstance use disorders.
(2) Advance cross-cutting research to prevent and treat OUD and overdoses in the context of chronic pain and other mental health conditions.
These research objectives incorporate other cross-cutting goals, including enhancing women’s and children’s health; addressing public health challenges across the lifespan; promoting collaborative science; and leveraging data science for biomedical discovery.
Within these core objectives are the following five research goals, each with associated specific aims:
- Develop and test novel prevention, treatment, and recovery strategies for OUD, other substance use disorders (SUDs), and overdoses.
- Advance research to prevent and treat polysubstance use disorders (PolySUD) and drug overdoses.
- Develop prevention interventions for high-risk populations impacted by the overdose crisis.
- Address treatment and recovery challenges associated with OUD co-morbidities and with polysubstance misuse.
- Integrate existing and newly generated data to advance data science in OUD and overdose, including for the identification of risk biomarkers, predictive models of treatment responses, and new -therapeutic targets.
Objective 1: Advance Research on the Prevention and Treatment of OUD and other SUDs that Contribute to Overdoses, and on Overdose Treatments
Effective prevention strategies can reduce the likelihood that individuals at risk for substance use begin to misuse opioids or other drugs and develop OUD or other SUDs that can lead to overdose. For those who do develop OUD or other SUDs, effective treatments are critical to reduce their risk of overdose. HEAL research strives to develop new or improved prevention and treatment strategies for OUD and other SUDs, including PolySUD. These interventions must be tailored to the severity of one’s overall risk and the range of settings in which they can be deployed.
Goal 1‐1: Develop and Test Novel Prevention, Treatment, and Recovery Strategies for OUD, Other SUDs, and Overdoses.
The cascade of care for addiction and overdose begins with primary prevention and proceeds through treatment into sustained recovery. Prevention, treatment, and recovery are all central to national and community-level efforts to address substance use and the serious risks associated with it, including disease, injury, overdose, and death. HEAL research will support the development and implementation of interventions across the continuum of care for individuals at all stages of life, including for adolescents at risk for opioid misuse and OUD.
Specific Aims:
- Develop, test, and implement evidence-based interventions and services aligned with the cascade of care for OUD and overdose, including prevention, treatment, and recovery support services.
- Develop interventions to detect and prevent prescription pill misuse (including counterfeit pills) among youth and the negative consequences associated with it, including overdoses.
- Develop interventions for adolescents with OUD, including mild OUD, and test the safety and efficacy of existing medications for opioid use disorder (MOUD) to treat moderate to severe OUD in this population.
- Streamline timelines for promising and accessible medications, devices, and other therapeutics for OUD and other SUDs (including therapies to reduce pain and novel abuse resistant opioid formulations) to advance through FDA approval.
- Support research to establish alternative endpoints to abstinence as treatment targets for OUD or other SUDs that contribute to overdoses, such as clinical endpoints that measure withdrawal, depression, craving, or use disorder severity.
- Support research to characterize long-term trajectories and outcomes for individuals with OUD including those associated with recovery and the factors that impact these outcomes.
- Analyze administrative federal and private data (i.e., Centers for Medicare & Medicaid Services, IQVIA) to understand geographical differences in treatment utilization for OUD, including access to MOUD, and develop dashboards to monitor regional needs and changes in real time.
Goal 1‐2: Advance Research on Prevention and Treatment of Polysubstance Use, Polysubstance Use Disorders (PolySUD) and Drug Overdoses.
In the past 10 years there have been significant increases in overdose deaths that involve combination of fentanyl with various drugs. Most notable are combinations of fentanyl with cocaine, and/or methamphetamine, which among all fatal drug combinations have shown the steepest increases.9 Drug dealers have increasingly mixed fentanyl with other illicit drugs in recent years, which expanded the pool of people who are at risk for overdosing and made it harder to reverse overdoses. Drug combinations also complicate the treatment of OUD and other SUDs, as the severe physical withdrawal from drugs like fentanyl and xylazine render MOUD harder to implement. Research is needed to develop interventions to prevent and treat polysubstance use and related overdoses.
Specific Aims:
- Support research on the mechanisms of toxicity of drugs, by themselves or in combination, including mechanisms of polysubstance overdose.
- Develop more sensitive and broadly accessible technologies for quantifying drugs in biological samples and for measuring the drugs present in confiscated drugs or drug use paraphernalia.
- Develop therapeutics for PolySUD, such as medication and neuromodulation approaches that address common targets (i.e., D3 receptors, GLP-1 receptors, orexin receptors) and/or circuits relevant to addiction irrespective of specific drug type. Such interventions could, for example, be targeted to strengthen self-regulation, buffer negative emotions, and/or modulate stress response among other goals.
- Develop therapeutics in addition to opioid antagonists for polysubstance overdoses, such as drug sequestrants, medications to stimulate the respiratory center, and devices for automatic respiratory stimulation.
- Explore health outcomes and drug misuse trajectories of individuals with polysubstance use including those with PolySUD.
Goal 1‐3: Develop Prevention Interventions for High-Risk Populations Impacted by the Overdose Crisis.
From its inception, the opioid overdose crisis manifested itself differently across geographic locations and demographic groups. Whereas overdose mortality rates were initially higher among White American men and women, particularly those living in rural or semirural areas, currently overdoses are highest among American Indian/Alaska Native American men and older Black American men. The factors contributing to these disparities have shifted as the drugs driving overdoses changed from opioid medications to heroin, fentanyl, and polysubstances. Common contributing factors in all the waves of the overdose epidemic are having a low-income or disability (including a mental disorder), lacking employment or housing, and having a history of incarceration.10
Specific Aims:
- Identify the key characteristics and approaches implemented by communities that have been able to reduce overdose death rates and apply those lessons learned to other communities.
- Utilize data, monitoring, technology, and Artificial Intelligence (AI) to identify and inform the deployment of interventions for populations at high-risk of opioid use and overdose.
- Increase inclusion of people with lived and living experience of substance use, especially those who are homeless and in law enforcement settings, in the research process.
Objective 2: Advance research to prevent and treat OUD and overdoses in the context of chronic pain and other mental health disorders
People with OUD and other SUDs are much more likely to have other medical conditions, including chronic pain and mental health disorders, than the general population. This comorbidity is associated with worse clinical outcomes both for OUDs and for the conditions with which they co-occur. The co-occurrence of opioid use and pain is a particular area of focus for the HEAL Initiative given the early role of prescription opioid misuse in driving the overdose crisis and the continued use of alcohol, cannabis and prescription opioids for pain relief.
Goal 2‐1: Address Treatment and Recovery Challenges Associated with Opioid Use Disorder Co-morbidities and with Polysubstance Misuse.
Managing OUD and co-occurring conditions can be especially challenging for healthcare providers. Treating PolySUD and other medical comorbidities requires carefully coordinated care. Indeed, depending on the conditions a patient is diagnosed with, healthcare providers may need to balance the prescription of necessary medications with risk of addiction to those same medications, as may be the case for patients with OUD and chronic pain. Therefore, treating OUD patients with medical comorbidities often requires a multidisciplinary approach that may involve addiction counselors, other mental health professionals, pain specialists, and other providers. Research is needed to develop optimal treatments and treatment delivery models for this population.
Specific Aims:
- Identify common neural circuits involved in OUD, pain, and mental health disorders.
- Evaluate the potential of existing therapeutics for conditions that share neural circuitry with OUD as OUD treatments. For example, evaluate the potential of GLP-1 agonist drugs used for treating diabetes and obesity for the treatment of OUD and PolySUD.
- Advance integrated models of care to address OUD and psychiatric and medical co-morbidities, including management of severe chronic pain in patients with OUD.
Goal 2‐2: Integrate Existing and Newly Generated Data to Advance Data Science in OUD and Overdoses, Including for the Identification of Risk Biomarkers, Predictive Models of Treatment Responses, and New Medication Targets.
HEAL will support research that leverages and integrates a variety of data sets including large-scale clinical data (such as from electronic health records (EHR), mortality records, and pharmacy dispensing databases) and tools to provide more accurate, real-time assessments on OUD, overdose and chronic pain management and its changing dynamics. Data should be accessible to inform targeted solutions for communities in need. HEAL researchers should make their data more findable, accessible, interoperable, and re-useable (FAIR), with the goal of fostering discovery and contributing to the HEAL Data Ecosystem.11
Specific Aims:
- Develop methods to capture data on opioid usage and emerging new substances on a real-time or near real-time basis.
- Improve technologies to mine or automatically extract data from EHR, clinical trial data, digital health devices, social media, and other observational and experimental data sources.
- Optimize clinical data standards to help advance AI and other research analysis tools toward addressing the challenges of OUD, overdoses and chronic pain management.
References
- https://www.ninds.nih.gov/current-research/trans-agency-activities/pain-consortium
- grants.nih.gov/grants/guide/notice-files/NOT-NS-24-106.html
- NCHS, Drug Overdose Deaths in the United States, 2003–2023
- www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- www.samhsa.gov/data/report/2023-nsduh-detailed-tables
- jamanetwork.com/journals/jamapsychiatry/fullarticle/2796749
- ajph.aphapublications.org/doi/full/10.2105/AJPH.2018.304673
- www.cdc.gov/mmwr/volumes/72/wr/mm7215a1.htm
- nida.nih.gov/research-topics/trends-statistics/overdose-death-rates#Fig6
- pmc.ncbi.nlm.nih.gov/articles/PMC6968850/
- https://heal.nih.gov/data/heal-data-ecosystem