Highlights
Image

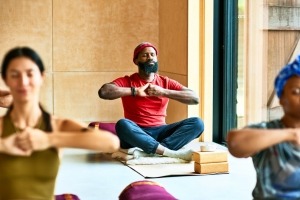
©Getty Images/FG Trade Latin
- The drug overdose and addiction crisis collided with the COVID-19 pandemic, with the potential to worsen the negative impacts of each for individuals. People who use drugs are more vulnerable to acquiring the virus that can cause COVID-19 and more likely to have worse health outcomes.
- However, the pandemic also led to opportunities for health care providers, substance use disorder recovery support systems, and other services to reach more people. For example, the U.S. government allowed flexibility for remote prescribing of buprenorphine and take-home dosing of methadone, medications used to treat opioid use disorder.
- NIDA conducts and supports research on the impacts of the COVID-19 pandemic on substance use and related health outcomes, and how the pandemic impacted adolescent health and brain development, including mental health and substance use. The institute is also researching sustainable, evidence-based strategies to overcome structural barriers to care.
Latest from NIDA
Reported drug use among adolescents continued to hold below pre-pandemic levels in 2023
|
New data show relatively low use of illicit substances, and yet overdose death rates among teens have risen
Overdose deaths involving buprenorphine did not proportionally increase with new flexibilities in prescribing
|
Federal study findings help understand effects of expanding access to treatment for opioid use disorder
The Federal Responses to the Drug Overdose Epidemic
|
The twin addiction and overdose crises have collided with the COVID-19 pandemic, each exacerbating the deleterious effects of the other
Find More Resources on COVID-19 and Substance Use Disorders
- Find a COVID-19 vaccine near you at Vaccines.gov.
- Read more information on COVID-19 risk and severity among people who use substances from the Centers for Disease Control and Prevention (CDC).
- Researchers: Find coronavirus COVID-19 information for NIH applicants and recipients of NIH funding.