Be it a condition of a job application or an addiction treatment program, a urine drug screen result can be life-altering. Stephanie Weiss’s research helps labs and clinicians use drug screening tools appropriately and interpret results correctly. A physician-scientist with a combined background in pharmaceutical chemistry, medical toxicology, emergency medicine, and addiction medicine, Dr. Weiss is a staff clinician in NIDA’s Intramural Research Program.
Q. Drugs aside—how much can be learned about someone from a urine sample?
Many times when doctors are checking patients’ urine, they’re not looking for drugs. My clinical background is as an emergency physician, and in that context, I was usually looking for an infection, blood, pregnancy—that kind of thing. Urine is often a quick and easy first screen for illness and unseen injury that can help people get the timely treatment they need.
Q. NIDA often hears from people who say their urine test came back positive for drug use, even though people are adamant that they didn’t use drugs. Can that story ever be true?
Absolutely. Initial urine drug screens frequently do produce what we call a “false positive.”
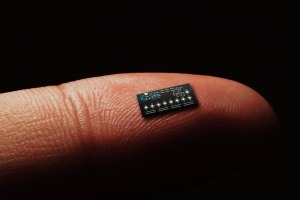
These screens use chemicals called antibodies to detect drugs at the molecular level. For a positive result, the test indicates that the antibody bound—like a very small lock and key—to a drug or one of its chemical derivatives. These non-invasive tests provide useful and rapid results, but the antibodies can sometimes be fooled and bind to other chemicals that are similar in shape to what they were supposed to detect. For example, a person may be taking a prescribed medication where the molecules have a similar shape to an illicit drug. In that case, the antibodies may cross-react, and the test is fooled into flagging it as a sign of drug use with a positive result.
Antibody tests that look for a whole class of drugs called amphetamines are particularly notorious for doing this. Clinicians, labs, companies, and others who test for drugs are aware false positives can happen, which is why more specific confirmatory testing is typically ordered when urine screens show a positive result.
It could even be a true positive with another explanation. Some people don’t realize that if you go to an ear, nose, and throat specialist, the doctor may administer a cocaine hydrochloride nasal solution during certain procedures. It’s a very effective vasoconstrictor (a medication that decreases bleeding by making the blood vessels contract). I used to use it on patients in the ER sometimes to stop nose bleeds. It works very well, but you do have to warn the patient that if someone tests them for cocaine for the next few days, they could test positive.
Q. So even true positives might not tell the whole story. What about environmental exposures? If someone walks through cannabis smoke outdoors, could that trigger a positive result in a urine screen?
This is something that's been studied extensively. If you are sitting in a small vehicle with all the windows rolled up, and a couple of people sitting in the car with you are smoking cannabis heavily, you may inhale secondhand smoke and could potentially test positive. That would again be a real positive even though you are not the person actually smoking. In terms of just walking by cannabis smoke outside, a positive result is unlikely. You would need to be exposed to a high enough concentration of THC— the primary psychoactive chemical in cannabis—for it to register on the test.
Q. What can someone do if they think they have received a false positive or have another explanation for their drug test results?
Sometimes a person’s explanation for why the test is positive differs from what the ordering physician or company is seeing on their test. Procedures may vary, but in many cases, a medical review officer can investigate the disputed result. These specially trained individuals will interview the patient to find out what other alternative explanations could be possible—because it's obviously a very bad thing to make an important decision with inaccurate information.
Note: NIDA is a biomedical research organization and does not provide personal medical advice, legal consultation, or medical review services to the public. Those with concerns about drug screening results may consider contacting the drug screening program for more information about medical review services. See NIDA’s Frequently Asked Questions for more information on interpreting drug test results.
Q. You published a case study that demonstrated why expert help to correctly interpret drug testing is sometimes needed. Tell us about that.
During my addiction medicine fellowship, I worked at an opioid treatment program, or OTP, that did periodic drug testing. OTPs are federally regulated clinics that provide medications to treat patients with opioid use disorder, including methadone or buprenorphine.
When one patient arrived, she reported that she had used fentanyl and tested positive, as expected. Three weeks later, the program did a repeat urine drug test that was again positive for fentanyl. Her doctor ordered a much more sensitive and specific type of confirmatory testing. That was also positive, so there were concerns that she had returned to use.
However, the patient adamantly denied using fentanyl since entering treatment. Her counselor and I believed her, so we got the confirmatory test results for her first urine sample to compare to the second results. The second fentanyl test was positive—but only for the chemical product the body breaks fentanyl down into, and only barely above the threshold of detection. If they had waited another day or two, she might have tested negative that second time.
What I think happened is that fentanyl is a very fat-soluble drug, so it dissolves in the body’s tissues and slowly leeches out—and the test was sensitive enough to pick that up. Fortunately, the lab had saved her initial urine sample, and comparing the confirmatory testing results from the two samples showed that this second positive test result could be explained by her fentanyl use three weeks prior—before she joined the treatment program. So we were able to show that the patient was telling the truth.
At the time this happened, it was not common knowledge that fentanyl byproducts can linger for several weeks in the urine. That’s why the patient gave me permission to publish the case. I said to her, “What happened to you is terrible and should never happen to anybody. I would like your help to educate other practitioners.”
My colleagues and I wanted to make sure that that other physicians, nurse practitioners, physicians’ assistants, and other people who take care of patients are aware that test results may stay positive for as long as a few weeks in people who used illicit fentanyl heavily or frequently. Now, I’m working with colleagues at NIDA to study how long patients’ urine can test positive for other drugs like cocaine and methamphetamine so that we can help clinicians learn to interpret those drug tests better also.
Q. If urine drug tests can be misinterpreted and produce false positives, why use them?
It's like a hammer, right? You could use it to hang up pictures. You could use it to build a house. In terrible cases, it can be a weapon. All tools, including drug tests, can be used in both good and bad ways. We want to improve how drug tests are used because they can be useful in some situations. Indeed, how physicians use this technology is changing. There are contexts where drug testing can be used as a therapeutic aid by opening conversation. Not to say “Gotcha!” to the patient, but to say, “Hey, your drug test result is not consistent with what you're telling me. I want to talk to you about this so I can understand what’s going on with you.” That discussion can lead to tailoring a treatment plan to better support that patient.
In fact, drug testing is key to certain types of treatment like contingency management, which involves giving people small rewards if they test negative for drug use. We also use drug testing during research to see if a potential treatment can help reduce or stop drug use.
Q. How can we improve the practice of drug testing? Is it a matter of clinician training, or do we need more science?
I would say we need both. Drug use is changing rapidly. We’re seeing more people exposed to new synthetic drugs—as well as very different patterns of substance use depending on the part of the country or world that you’re in. But researchers, clinical chemists, and medical toxicologists work together on these challenges. That may mean developing new screening technology or sharing information on testing for emerging and less-familiar drugs. Organizations that help with that communication—like the National Drug Early Warning System, which NIDA funds—inform and are informed by drug testing.
In terms of training, medicine is now super specialized. It's not possible for one person to know everything. I would tell general practitioners that they can phone a friend and make use of their consultants. Every lab at a hospital or clinic is run by a clinical chemist with a Ph.D., and these people are specially trained in how to conduct and interpret lab testing. At academic centers, clinicians may also be able to consult a medical toxicologist. These are physicians with specialized training in poisonings and overdoses who can help the care team understand how a patient’s test results relate to their clinical presentation. All of these folks can help improve interpretation.